By definition, ‘accessible’ means being reached or is within reach, as well as the capability of being used, seen, understood, or appreciated. A few common examples of this applied in society include ramps for individuals that navigate the world in a wheelchair, iPhone’s VoiceOver screen reader for people that have a vision impairment or color blindness, and vibrating street crossing buttons to alert those with both hearing and vision loss. Accessibility creates an environment where being an able-bodied individual is not the only standard from which the universe operates. It is all-inclusive, modifying what is already available and always expanding to give everybody the best chance at a successful life not determined by their disability or circumstances. Massage and bodywork, alternative medicine, body movement therapies such as yoga or Tai Chi, and self-care practices and education should be accessible by everyone. In the case of those who are homeless, living in poverty, or are low income, there are many barriers that can stand in the way of them receiving this care, cost, and knowledge being at the top of the list. This paper will discuss the physical and mental effects of being homeless or living in poverty, the positive effects of complementary alternative medicine in this population and why it is vital they receive it regularly, as well as what actions are currently being taken to address the issues of accessibility of this care and why it should matter to you.
According to the United States Census Bureau, in 2017 thirty-nine million people (12.3%) in the United States were living in poverty and almost four-hundred thousand of those people were San Diego residents (11.9%.) Poverty is measured by the U.S. Census Bureau using set income thresholds that vary based on the composition and size of a family. If that family’s income totals less than their threshold value, they are considered as living in poverty. In 2017, the computed poverty threshold for one person living in the United States was 12,488 dollars. With the average population per household being 2.54 that same year, two adults and one child, the poverty threshold was 19,515 dollars. In stark comparison, the median household income of the U.S. in 2017 was 61,372 dollars. Poverty is not just struggling to pay bills or missing a meal, chronic poverty puts physical, emotional, and mental stress and pressures on millions of families each year. The effects of poverty are generational and cyclical, and they extensively impact individuals of all ages, races, and ethnicities nationwide. The basic necessities of survival such as food, shelter, and clean drinking water become such a struggle to secure that things like healthcare, education, and entertainment are seen as frivolous luxuries. Children born into and developing in poverty have higher rates of delinquency, depression and anxiety disorders, lower academic scores, and higher prevalence of cognitive, attention, and behavioral problems. Poverty in adulthood is host to the development of numerous mental health disorders, physiological and psychological stress, and higher rates of suicide. Where there is poverty, there is a lack of education, crime, joblessness, and poor physical and mental health.
In a study published in 2015 done in partnership between San Francisco State University’s Institute for Holistic Health Studies, the National Center for Complementary and Integrative Health, and Texas Tech University Health Science Centers, a direct correlation was found between level of education/income level and knowledge or lack of knowledge of 4 common complementary health practices. A correlation was also discovered between the level of education and ‘lack of need’ being a reason for not utilizing those complementary health approaches. During this research, a survey was used to poll people who have never used acupuncture, chiropractic work, supplements, and herbs, or yoga and their reasoning why. Those who did not graduate from high school were 29-58% more likely to have selected ‘lack of knowledge’ as a reason for non-use across all categories polled. Individuals with higher income levels polled less likely to select ‘lack of knowledge’ as a reason of non-use, for example, this bracket was 37% less likely to choose ‘lack of knowledge’ as a reason for not using chiropractic care. On the basis of education, voters with a higher level of completed education were significantly more likely to choose ‘lack of need’ as a response to non-use of complementary health. Those who attended college were 22% more likely to select ‘lack of need’ in response to non-use of chiropractor and acupuncture care. In conclusion, this data coincides perfectly with the sentiments mentioned above. Living in poverty drastically diminishes the opportunity for affording educational opportunities and utilizing healthcare services. It can be inferred from above that having a higher income equals better healthcare, less labor-intensive work, and potentially fewer injuries, thus creating less need for complementary health approaches.
A study published in 2016 by the U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, and the National Center for Health Statistics further prove the disparities between income level, access, and use of complementary health approaches. Families with incomes over one-hundred thousand dollars had four times more out-of-pocket expenses ($6.2 billion) paid for visits to complementary health practitioners per year than those families making less than twenty-five thousand dollars (1.3 billion.) Natural products and supplement sales paid for out-of-pocket per year were twice as much for families with incomes between fifty and ninety-nine thousand dollars ($4.1 billion) than for those making less than twenty-five thousand dollars ($1.9 billion.) Furthermore, individuals in two of the highest income brackets spent significantly more than half of all the out-of-pocket expenditures for complementary health approaches ($21.1 billion/70.2%.) Those families were also willing to spend almost one-hundred and sixty dollars more on average per occasion while receiving complementary healthcare services or purchasing health products. These studies draw two main conclusions, higher-income individuals, overall, are either spending the most amount of money on alternative healthcare or have the knowledge and means to use it but do not feel the need to. While those with lower incomes and/or living in poverty contribute significantly less money to the purchases of alternative healthcare, the population even more vulnerable and most often forgotten in the world of complementary health services is homeless.
According to The 2018 Annual Homeless Assessment Report (AHAR) to Congress, over half a million people nationwide experience homelessness on any given night. Half of all homeless individuals reside in the top five states with the highest rates of homeless populations. California has the most total people experiencing homelessness at almost one-hundred and thirty thousand homeless individuals any given day, followed by New York, Florida, Texas, and Washington. 2019’s WeAllCount, point-in-time-count, San Diego results show at the very minimum, just over eight-thousand San Diegans live on the streets or shelters on any given night, making it fourth highest on the list of major cities with the most occurrence of homelessness. Thirty-six percent, of the homeless population in San Diego, report being physically disabled, twelve percent are under the age of twenty-four, ten percent are veterans, and three percent are families with at least one child. The effects of homelessness are much more extensive and physically dangerous than those effects of individuals living in poverty. The homeless experience more serious health conditions such as skin diseases due to decreased hygiene habits and access to clean running water, cold or heat injuries by constant exposure to the elements, nutritional deficiencies due to poor diet and/or starvation, drug dependency, alcoholism, mental illness, HIV/AIDS, and much higher rates of mortality, among many others. Psychological effects of homelessness include loss of self-esteem and self-worth, loss of ability and will to care for oneself, increased danger of abuse and violence, increased risk of taking part in or witnessing criminal activity and being incarcerated or otherwise being institutionalized, and development of behavioral problems including substance abuse.
The homeless population and those living in poverty are subjectively in the most need of massage and bodywork, alternative medicine, body movement therapies, and self-care instruction and education, but are least likely to have access to it, let alone be able to engage in it. These types of therapies have the potential to be highly effective for reducing stress and anxiety, increasing blood flow and lymphatic drainage, lowering blood pressure, and soothing neuromuscular pain and discomfort. Such treatments are less expensive long term due to the focus being preventative, this can lead to fewer injuries and illnesses, fewer doctors’ visits and less reliance on prescription medication. High prices and the fight of getting insurance companies to cover complementary health prevents access to these alternatives for many low-income Americans and most of the homeless population.
A 2008 issue of Healing Hands, a publication of the Healthcare for the Homeless (HCH) Clinicians’ Network, explored the use of complementary and alternative therapies in homeless healthcare. HCH Manchester in New Hampshire developed an eight-week long training program working to educate and teach the homeless population ‘Mindfulness-Based Stress Reduction’ (MBSR.) The program consists of two to three hour-long sessions once a week focusing on mindfulness meditation and yoga practices, with a full-day retreat scheduled in week six. Also on staff are a psychologist, social worker, and substance abuse counselor that are available at any time to better assist the participants. To track results, they use a quality of life survey before and after completion of the program to document perceived improvements. Outcomes include reduced pain and increased ability to cope with chronic pain, increased abilities in dealing with stressors and being able to relax, increased sense of well-being and enthusiasm for life, and improved self-esteem, clarity, and awareness. In addition to this program, HCH Manchester also offers clinic services including medical and mental health care, addiction counseling, health education, social services, assistance with food stamps, Medicaid, and disability services, and dental and eye care. For those who are homeless or living in poverty, you are always in fight-or-flight and survival mode. Getting a chance to think clearly, feel safe, cry, laugh, and feel emotions, and even just a kind word or gentle touch can mean the world to them. Everyone deserves the opportunity to feel human and to feel cared for.
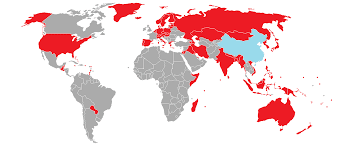
Many organizations across the nation are realizing the need for alternative health for the homeless, low income, and improvised populations. New York Harm Reduction Educator works to put drug users and sex workers on the path of recovery, by providing syringe exchange, education, and outreach services. Other services include overdose prevention, counseling and family stabilization services, STD testing, support groups, sex education, as well as holistic health services. NYHRE provides meditation, reiki, qi gong, breathing exercises, and ear acupuncture throughout the city at several of their street-based syringe exchanges. The Care Through Touch Institute in San Francisco, California gives free chair massage at various shelters and churches, to the community of people who experience homelessness or are marginally housed. They also have a program called Comfort, Care, & Companioning Program that targets homeless and marginally housed seniors. This program provides a companion to give comforting massage, caring conversation, and companionship to support these individuals dealing with isolation and physical and emotional pain related to conditions arising from the aging process or illness and injury. Last but certainly not least, Everytable, a restaurant with a fast-food style twist, makes healthy foods quick and accessible to underserved communities in Los Angles, California. The meals are priced according to the neighborhood they serve, making them affordable to lower-income individuals and those living in poverty. The meals are healthy, fresh, and made from scratch and provided to communities with limited or no access to affordable healthy foods and sold at discounted prices.
While there are people out there doing great things and making big strides in creating more accessibility of complementary alternative medicine to vulnerable populations such as the poor and homeless, we still have a long way to go. Education and advocacy are the most critical aspects. Education of the health professionals and practitioners and education of those in need, as well as continually advocate for affected individuals and striving to make positive changes.
Works Cited
Allen, DMD, J., Carlson, APRN, BC, T., Colangelo, LSW, B., Orman, S., Rabiner, MD, M., Rodriguez-marzec, MS, FNP-C, PMHNP-C, R., . . . Bredensteiner, S. (2008, June). Healing Hands: Use of Complementary & Alternative Therapies in Homeless Health Care (P. Post, MPA, Ed.). Retrieved July, 2019, from www.nhchc.org/wp-content/uploads/2011/09/jun2008HealingHands.pdf
Burke, A., Nahin, R. L., & Stussman, B. J. (2015, June 17). Limited Health Knowledge as a Reason for Non-Use of Four Common Complementary Health Practices. Retrieved July, 2019, from www.ncbi.nlm.gov/pmc/articles/PMC4470691/#_ffn_sectitle
Care Through Touch Institute. (n.d.). Carethroughtouch.org. Retrieved July, 2019, from www.carethroughtouch.org/welcome
CMC Catholic Medical Center. (n.d.). Health Care for the Homeless Program Manchester. Retrieved July, 2019, from www.catholicmedicalcenter.org/care-and-treatment/community-health/health-care-for-the-homeless
EVERYTABLE. (n.d.). Everytable.com. Retrieved July, 2019, from www.everytable.com/mission/
Fontenot, K., Semega, J., & Kollar, M. (2018, September). Income and Poverty in the United States:2017. Retrieved July, 2019, from www.census.gov/content/dam/Census/library/publications/2018/demo/p60-263.pdf
Henry, M., Mahathey, A., Morrill, T., Robinson, A., Shivji, A., & Watt, R. (2018, December). The 2018 Annual Homeless Assessment Report (AHAR) To Congress. Retrieved July, 2019, from files.hudexchange.info
Nahin, Ph.D., M.P.H., R. L., National Institutes of Health, Barnes, M.A., P. M., National Center for Health Statistics, & Stussman, B.A., B. J. (2016, June 22). National Health Statistics Report: Expenditures on Complementary Health Approaches: United States, 2012. Retrieved July, 2019, from www.cdc.gov/nchs/data/nhsr/nhsr095.pdf
New York Harm ReductionEducators. (2019). Nyhre.org. Retrieved July, 2019, from nyhre.org/programs-services/holistic-health-services/
Simon, MD, K. M., Beder, MD, M., & Manseau, MD, MPH, M. W. (2018, June 29). Addressing Poverty and Mental Illness. Retrieved July, 2019, from www.psychiatrictimes.com/special-reports/addressing-poverty-and-mental-illness
United States Census Bureau. (n.d.). Poverty: How the Census Bureau Measures Poverty. Retrieved July, 2019, from www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html
United States Census Bureau. (2010-2018). QuickFacts San Diego County, California; California. Retrieved July, 2019, from www.census.gov/quickfacts/fact/table/sandiegocountycalifornia,CA/PST045218
United States Census Bureau. (2017). Poverty Thresholds for 2017 by Size of Family and Number of Related Children Under 18 Years. Retrieved July, 2019, from www2.census.gov/programs-surveys/cps/tables/time-series/historical-poverty-threshold/thresh17.xls
United States Census Bureau. (2018, November). Average Population Per Household and Family: 1940 to Present. Retrieved July, 2019, from www2.census.gov/programs-surveys/demo/tables/families/time-series/households/hh6.xls